Abstract
The 2016 WHO classification recognized pre-fibrotic primary myelofibrosis (pre-PMF) as a distinct entity. However, little is known about the clinical characteristics and prognosis of pre-PMF patients with JAK2V617F mutations, CALR exon 9 mutations, and triple-negative (TN) mutations. Thrombotic prognostic model specific for pre-PMF is still lacking and the applicability of International Prognostic Score for Thrombosis in Essential Thrombocythemia (IPSET-thrombosis) needs further validation in pre-PMF patients.
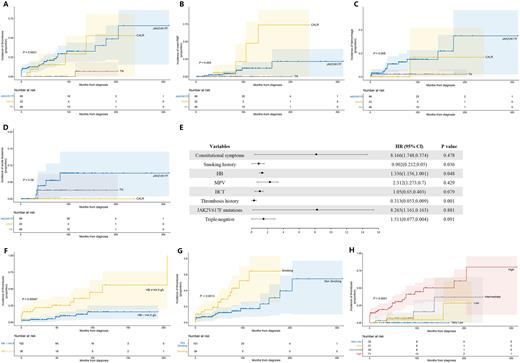
We conducted a retrospective study of 168 pre-PMF patients defined by 2016 WHO diagnostic criteria in the First Affiliated Hospital of Zhejiang University School of Medicine and the Fourth Affiliated Hospital of Zhejiang University School of Medicine (ChiCTR2200061208). We retrospectively evaluated the clinical characteristics, prognosis of hemorrhage and thrombosis, and the evolution risk to overt-PMF and acute leukemia in 168 pre-PMF patients. We also assessed the risk factors for thrombosis events and validated the availability of IPSET-thrombosis scoring system in pre-PMF patients. Among 168 pre-PMF patients, 98 (58.3%) harbored JAK2V617F, 22 (13.1%) CALR and 2 (1.2%) MPL mutations; 46 (27.4%) patients were negative for all three mutations. Compared to JAK2V617F-mutated cases, TN pre-PMF patients were younger (P<0.001), had fewer constitutional symptoms (P=0.003), lower white blood cell count (WBC) (P=0.01), hemoglobin level (HB) (P=0.007), mean platelet volume (MPV) (P=0.03), hematocrit value (HCT) (P=0.045), red blood cell distribution width (RDW) (P<0.001) and lactic dehydrogenase (LDH) (P=0.021). They also had fewer thrombotic events (1, 2.2%) compared to JAK2V617F group (25, 26.3%) and CALR group (5, 22.7%) during the follow-up and at diagnosis (P<0.001) (Figure A). A proportion of 7.1% and 18.2% progressed to overt-PMF in JAK2V617F and CALR group, respectively, while no TN pre-PMF patients developed overt-PMF progression (0, 0.0%) (P=0.015) (Figure B). We also found, although not statistically significant, a lower incidence of hemorrhagic events (2% vs. 12%) and acute leukemia (2% vs. 5%) in TN pre-PMF groups compared with JAK2V617F pre-PMF groups (Figure C, Figure D). As for risk factors for thrombosis, univariable analysis found thrombosis was associated with constitutional symptoms (P=0.003), thrombosis history (P<0.001), smoking status (P=0.007) and JAK2V617F mutations (P=0.008). Patients with higher HB (P=0.013), MPV (P=0.042) and HCT (P=0.040) were also more likely to develop thrombotic events. In multivariable analysis, smoking history (P=0.036; HR 0.902, 95% CI 0.05-0.212), higher HB value (P=0.048; HR 1.336, 95% CI 1.001-1.156) and thrombosis history (P=0.001; HR 0.313, 95% CI 0.009-0.053) had negative impact on the development of thrombosis events (Figure E). When divided by HB value with cut-off point of 144.5, subjects with HB value <144.5 g/L were less likely to develop thrombosis events compared to ≥144.5 g/L (P=0.003) (Figure F). And subjects with no history of smoking were less likely to develop thrombosis events compared to subjects with a history of smoking (P=0.004) (Figure G). We also validated IPSET-thrombosis scoring system in pre-PMF patients, results showed significant statistical difference among very low-, low-, intermediate- and high-risk groups (P<0.001) (Figure H).
In conclusion, TN pre-PMF patients were younger, had fewer constitutional symptoms, lower WBC, HB, MPV, HCT, RDW and LDH, and less likely to develop thrombotic events and overt-PMF compared to JAK2V617F and CALR groups. TN pre-PMF patients with smoking history, higher HB and thrombosis history had higher risks of thrombosis events. And IPSET-thrombosis scoring system was applicable in stratifying thrombosis risks of pre-PMF patients.
Acknowledgment: The research was supported by the Key R&D Program of Zhejiang, No. 2022C03137; Public Technology Application Research Program of Zhejiang, China, No. LGF21H080003; the Key Project of Jinhua Science and Technology Plan, China, No. 2020-3-011; the 2019-2022 Key Medical Discipline (Hematology) Fund of Jinhua, China.
Correspondence to: Dr Jian Huang, Department of Hematology, The First Affiliated Hospital of Zhejiang University School of Medicine.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal